Super User
Flat Feet
A flat foot is a foot that has no visible arch in the middle of the sole of the foot while standing. There are two types of flat feet. A flexible flat foot has a visible arch when the foot is not bearing weight, but the arch disappears when the person stands or puts any weight on the foot. A rigid flat foot has no visible arch regardless of whether or not the foot is bearing any weight. Flat feet can also be present from birth or can develop over time, as the ligaments that hold up the arch of the foot weaken. When flat feet are acquired, they are referred to as fallen arches.
In many cases, flat feet do not cause any pain or other symptoms. This is especially true for those who were born with flat feet. In the instances where flat feet are not asymptomatic, they may cause pain in the heel, arch, ankle, or along the outside of the foot, as well as shin pain, foot aches or fatigue, and lower back, hip, or knee pain. People who have flat feet are also more likely to have an abnormal gait or walking pattern that may affect their daily activities.
Flat feet can be diagnosed through a physical examination. An imaging study, such as an X-ray, may be used to determine the severity of the condition. Treatments for flat feet include footwear and activity modifications, wearing orthotics, taking medications to relieve pain, and physical therapy. If you have flat feet that are causing you pain or discomfort, please consult with a chiropodist.
How a Chiropodist Can Help With Your Feet

Seeking the expertise of a chiropodist can yield numerous benefits that contribute to overall health and comfort for your feet. Chiropodists are trained in theoretical, clinical, and practical aspects of foot and ankle disorders. They play a vital role in addressing a range of foot health issues, including flat feet, bunions, heel and arch pain, nail fungus, warts, and diabetic foot conditions. They also can provide personalized recommendations for custom footwear and orthotics, enabling patients to alleviate specific foot conditions. During your visit to a chiropodist, be prepared to discuss your medical history, which helps this medical professional to fully understand your condition. Today's leading chiropodists are committed to delivering optimal foot care, and promoting overall well-being. Complying with lifestyle modifications and recommendations from a chiropodist can expedite the recovery process, enabling you to embrace improved foot health and enhanced quality of life. If you have specific foot problems, it is suggested that you make an appointment with a chiropodist for treatment and guidance.
If you have any foot or ankle concerns, contact one of the chiropodists of The Footcare Centre. Our chiropodists can provide the care you need to keep you on your feet.
A chiropodist is a healthcare professional that specializes in the feet, ankles, and lower limbs. With the amount of work the feet do in a lifetime, the whole body works better if the feet are properly supported. Chiropodists must have a bachelor’s degree in science and complete a three to four-year chiropody program. They can then work independently or as part of a team. Chiropodists are like podiatrists, the only difference being the country they obtained where they obtained their degrees. The field can be called podiatry in the United States and chiropody elsewhere. A chiropodist is a popular term for this profession in the UK and Canada. Chiropodists treat a variety of foot problems from corns and calluses to fungal infections. Some also offer orthotics. They might provide a variety of foot therapies, injections, and surgical procedures. Normally one sees a chiropodist when they are experiencing pain but visiting one regularly, as one would a dentist, can help ensure the feet are in top form and help prevent future problems. If you suffer from foot or ankle pain or have questions about your lower extremities, book an appointment with a chiropodist today.
What Does a Chiropodist Do?
A chiropodist helps people with problems with their feet and ankles with the goal of making their lives more comfortable. A chiropodist takes care of blisters, corns, bunions, cracked heels, nail problems, and sprained ankles, just to mention a few things that can go wrong with our feet. A chiropodist will take your medical history and examine your feet for blood circulation and any other problems going on. They will watch you walk and how you move when you walk. They will discuss any findings they come up with and discuss a treatment plan with you.
What Does It Take to Become a Chiropodist?
Chiropodists must have seven to eight years of post-secondary school before beginning to practice. They must obtain a bachelor’s degree in science and complete a three-to-four-year chiropody program. Chiropodists work independently or as part of a team.
If you have any questions please feel free to contact our office located in Niagara Falls, ON . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Chiropodists
A chiropodist is a highly trained healthcare professional that provides the assessment, treatment, and management of chronic or acute foot and ankle problems. They aid in the prevention of injuries and disabilities and promote proper foot health for overall well-being. With foot problems being as prevalent as they are, the fact that the feet are the body’s foundation, and the necessity of keeping our feet as healthy as possible, chiropodists are needed to help with prevention, assessment, and treatment of issues that may arise with feet. When the feet are properly supported, the whole body works better. Chiropodists must have seven to eight years of post-secondary school before beginning to practice. They must obtain a bachelor’s degree in science and take a three to four year chiropody program. Chiropodists work independently or as part of a team. Chiropodists treat a variety of foot problems including bony foot deformities, corns, calluses, warts, fungal infections, nail conditions, and biomechanical dysfunctions. These healthcare providers also recommend or provide orthotics and insoles. They might also provide physical therapy, surgical procedures, injection administration, prescriptions, and various other therapies. Normally one sees a chiropodist when they are experiencing pain. However, visiting one regularly, as one would a dentist, can help ensure the feet are in top form and will help prevent future problems. If you suffer from foot or ankle pain or have questions about your lower extremities, book an appointment with a chiropodist.
Sever’s Disease and Heel Pain
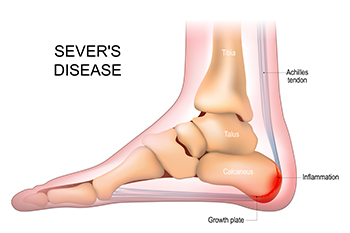
Sever's disease, also known as calcaneal apophysitis, is a common source of heel pain in physically active young individuals, typically emerging during puberty. It occurs more frequently in boys than girls and has no known single cause but likely results from factors like overuse and increased body weight. This condition involves the Achilles tendon's attachment to the heel bone, which is still in the process of changing from cartilage to bone in pre-teens. Symptoms include heel pain during physical activity, worsened pain after exercise, limping, and tiptoeing. Several factors contribute to Sever's disease, including changes in height, weight, increased physical activity volume, type of activity, and footwear choices. Treatment varies based on the level of pain and may include activity modification, load management, heel raises, orthotics, and time for the condition to improve. If your child has heel pain, it is suggested that you make an appointment with a chiropodist for a proper diagnosis and treatment options.
Sever’s disease typically affects young children and teenagers. If your child complains of foot pain, please consult with one of the chiropodists from The Footcare Centre. Our chiropodists will assess your condition and provide you with quality foot and ankle treatment.
What Is Sever’s Disease?
Sever’s disease, also known as calcaneal apophysitis, is an inflammation of the growth plate in the heel bone. It is typically caused by overuse due to repetitive activities such as running, jumping, and playing certain sports. This condition most frequently affects children between the ages of 8 and 14.
Symptoms
Symptoms of Sever’s disease include:
Pain in the back or bottom of the heel
Pain when the sides of the heel are squeezed
Limping or walking on tiptoes to avoid putting pressure on the heel
Difficulty running, jumping, or participating in usual activities
Fatigue
Diagnosis
Sever’s disease is diagnosed by taking a thorough medical history and performing a physical examination. Imaging studies, such as an X-ray, can help rule out other injuries like a fracture.
Treatment
Sever’s disease typically heals without any long-term complications. Treatment involves resting the affected foot by reducing typical activities, wearing orthotics to support the foot, immobilizing the affected foot, taking medications to reduce pain and inflammation, and stretching the foot.
If you have any questions, please feel free to contact our office located in . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Sever's Disease
Sever’s disease, also known as calcaneal apophysitis, is a foot condition that occurs in children. Sever’s disease is not truly a disease, but rather an overuse injury. It is common among active children between the ages of 8 and 14. Young, growing children have a growth plate in their heels, where new bone is forming. When too much stress is put on the heel, the growth plate can become inflamed, leading to heel pain.
Children who participate in activities that put repetitive stress on the heel bone are most at risk of developing Sever’s disease. These activities include playing soccer or basketball, running track, or any other sport or activity that involves running, jogging, or jumping. Children who are obese, have tight Achilles tendons, biomechanical problems, flat feet, or fallen arches are also at risk.
The symptoms of Sever’s disease include pain in the back or bottom of the heel, pain when the sides of the heel are squeezed, and fatigue. The pain may lead to difficulties walking or bearing weight on the affected foot, and you may notice your child limping or walking on their toes to avoid putting pressure on the heel. A chiropodist can diagnose Sever’s disease by taking a medical history and performing a physical examination. Imaging studies such as X-rays may also be ordered.
Sever’s disease is generally treated by resting the affected foot, wearing shoes or orthotics that support the heel, and taking nonsteroidal anti-inflammatory medications to reduce pain and inflammation. In severe cases of heel pain, the affected foot may need to be immobilized with a cast while it heals. If your child is complaining of heel pain, please consult with a chiropodist.
Causes of Foot Stress Fractures

Foot stress fractures, which are hairline cracks in the bones of the foot, can often bring athletic activity to a halt. Stress fractures, primarily a result of repetitive strain, stem from several factors. The key trigger for foot stress fractures is the excessive force applied to foot bones during rigorous activities, such as running, jumping, and fast-paced sports. The foot's repetitive impact on hard surfaces initiates the problem, making runners, football players, and gymnasts highly susceptible. Despite the seemingly tiny nature of these fractures, they can lead to immense pain and discomfort. Inadequate muscle support also plays a role in foot stress fracture formation. When individuals rapidly escalate their activity levels, such as taking up a new sport or intensifying training, the muscles may lack the necessary strength and endurance to support it. This deficiency compromises the support of the foot bones, resulting in an overload of force onto them. This then can lead to small cracks forming within the bones. If you believe you have developed stress fractures in your feet, it is suggested that you consult a chiropodist for an exam and treatment options.
A stress fracture often requires medical attention as it can progress and worsen over time. Please consult with one of the chiropodists from The Footcare Centre. Our chiropodists will assess your condition and provide you with quality foot and ankle treatment.
A stress fracture refers to a fine crack in a bone. This type of fracture is especially common in the feet, as they often endure repetitive pressure from daily activities such as walking or running. Stress fractures occur when the affected bone can not support the load being placed on it. Stress fractures in the foot can occur in any bone, but often affect the metatarsal bones which connect the toes to the rest of the foot, the heel bone, or the navicular bone on the top of the foot.
Symptoms
Symptoms of a stress fracture may include:
Deep, dull pain
Sharp, localized pain
Intermittent pain
Tenderness
Weakness
Swelling
Bruising
Changes in the biomechanics of the foot
Diagnosis
Stress fractures in the foot are diagnosed via medical history and a physical exam. You may also need to have diagnostic imaging tests like X-rays, MRIs, CT scans, bone scans, or an ultrasound performed to confirm the diagnosis and to rule out any other problems.
Treatment
Nonsurgical treatment options include resting, icing, compressing and elevating the affected foot, taking nonsteroidal anti-inflammatory pain medications, modifying your footwear, wearing a cast, and using crutches. Certain types of foot fractures, such as navicular fractures, respond poorly to nonsurgical treatment and may need surgery to fully heal.
If you have any questions, please feel free to contact our office located in . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Tired, Achy Feet

Tired and achy feet, while not a medical condition in and of itself, often result from overworked foot muscles. Our feet endure substantial pressure and movement, causing fatigue. This sensation can affect daily activities and slow us down. Various factors contribute to tired and achy feet. Overuse, such as prolonged standing or walking, is a significant cause. Inadequate footwear, especially lacking arch support and cushioning, can lead to foot discomfort. Walking on hard surfaces, high or fallen arches, excess weight, and foot conditions like heel spurs or plantar fasciitis can intensify these feelings. Relief and prevention of tired and achy feet can include rest, foot soaks, massage, stretching and strengthening exercises, and wearing shoes with adequate arch support and shock absorption with insoles or orthotics. If you have tired, achy feet, it is suggested that you make an appointment with a chiropodist to see if the underlying cause can be identified and treated.
Foot pain is a common problem treated by chiropodists. If you have foot pain, please consult with one of the chiropodists from The Footcare Centre. Our chiropodists can help you maintain the health of your lower limbs and your mobility.
When you are experiencing foot pain, it’s important to note the type of pain and its location, as this can help determine a diagnosis.
Pain in the top of the foot may be caused by:
Stress fractures
Sinus tarsi syndrome
Extensor tendonitis
Tibialis anterior tendonitis
Gout
Athlete’s foot
Ganglion cysts
Pain in the bottom of the foot may be caused by:
Plantar fasciitis
Foot cramps
Tarsal tunnel syndrome
Plantar fibromatosis
Posterior tibial tendonitis
Stress fractures
Flat feet
Pain on the side of the foot may be caused by:
Ankle sprain
Cuboid syndrome
Peroneal tendonitis
Stress fractures
Bunions
Corns or calluses
Posterior tibial tendonitis
Heel pain may be caused by:
Plantar fasciitis
Achilles tendonitis
Bone spurs
Heel fractures
Retrocalcaneal bursitis
Sever’s disease
Pain in the toes may be caused by:
Gout
Hammertoe
Turf toe
Bunions
Ingrown toenails
Blisters
Arthritis
These and many more conditions can be treated by a chiropodist. If you have any questions, please feel free to contact our office located in . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
If you’re suffering from foot pain, it’s important to note the locations and quality of your foot pain. Pain can affect any part of the foot, including the top, bottom, side, heel, or toes. The pain may be sharp, stabbing, dull, achy, burning, or stinging, and can come on suddenly or develop gradually over time.
Pain in the top, bottom, or side of the foot can have many causes. In addition to the type of pain and its location, it’s also important to note when the pain started, what you were doing at the time, and what aggravates the pain. For example, pain in the top of the foot that worsens with physical activity or weight-bearing, that has gradually gotten worse over time, and is accompanied by swelling and tenderness could be indicative of a stress fracture.
Pain in the heel is a frequent concern, especially among patients who participate in sports, run, or wear high heels. Plantar fasciitis, an inflammation of the ligament that runs along the bottom of the foot and connects the heels to the toes, can cause stabbing heel pain. The pain is usually at its worst upon taking your first few steps in the morning or after a long rest and can radiate to the arch of the foot. Plantar fasciitis is also often associated with heel spurs, bony outgrowths on the heel bones that can be painful if they poke into the surrounding tissues.
Foot pain can be caused by not only injuries but also problems with the biomechanics of the feet and underlying health problems, like diabetes or peripheral neuropathy. If you’re experiencing foot pain, please seek the care of a chiropodist near you.
The Difference Between Bunions and Gout

Bunions and gout share similarities in their impact on the big toe. Both are characterized by pain, swelling, and redness, often leading to walking discomfort. However, they possess fundamental differences in origin and treatment. Bunions are localized foot deformities, while gout is a systemic issue resulting from excessive uric acid production. Bunions arise from genetic or structural foot anomalies and are impacted by footwear, while gout stems from hyperuricemia triggered by purine-rich foods. The location, sensation, and causes of each condition diverge. Bunions appear as bony protrusions at the big toe joint, while gout predominantly affects the big toe but also other joints. Gout attacks involve excruciating pain, heat, and tenderness, while bunions cause discomfort through structural changes. Diagnosing these conditions involves various tests, with gout requiring a more extensive evaluation to rule out similar conditions. Gout is confirmed through medical history, physical examination, uric acid blood tests, joint aspiration, and imaging. Bunion diagnosis involves physical assessment and X-rays. Gout management focuses on acute attack relief through lifestyle changes and medications to control uric acid levels. The initial treatment of bunions includes wearing proper footwear, taping, and arch supports. If you are having pain or discomfort in your big toe, it is suggested that you make an appointment with a chiropodist for a proper diagnosis and appropriate treatment.
Bunions progressively worsen over time and may cause walking in your shoes to become difficult. To learn more about bunions, please consult with one of the chiropodists from The Footcare Centre. Our chiropodists will assess your condition and provide you with quality foot and ankle treatment.
What Are Bunions?
A bunion is a bony bump that protrudes from the base of the big toe. Bunions are caused due to a misalignment of the first metatarsal. The characteristic bump of a bunion forms when the metatarsal shifts outwards from its proper position. Bunions develop slowly over time and progressively worsen without treatment. The skin over the bunion may develop calluses due to the friction from shoes. Eventually, a bunion can make walking uncomfortable or even painful. Bunions are one of the most common foot deformities and are especially common in women and older adults.
Symptoms
A bunion appears as a bulging bump on the outside of the base of the big toe.
The bunion may also:
Be swollen, red, or sore
Develop corns or calluses over it
Cause pain
Limit the big toe’s range of motion
Treatment
There are several different treatments available for bunions. Conservative treatment options include wearing shoes with a wider toe box, cushioning the bunion with a specialized pad, wearing shoe inserts, icing the bunion if it becomes inflamed, and taking medications to relieve pain. In more severe cases, more invasive procedures may be done. This may involve removing the swollen tissue around the bunion, straightening the big toe, realigning the bones at the front of the foot, or a combination of these procedures.
If you have any questions, please feel free to contact our office located in . We offer the newest diagnostic and treatment technologies for all your foot care needs