Super User
Obesity and the Feet
Obesity can affect the feet in a variety of ways. Your feet bear the weight of your body, carrying you through life. When the feet are under immense strain from excess weight, they are more prone to both chronic and acute injuries. Over time, the pressure from excess weight can cause the feet to flatten and widen as the arches of the feet slowly collapse. This can not only increase your shoe size, but also lead to foot pain, difficulty walking, and a dysfunctional gait or walking pattern. A variety of foot and ankle injuries are common in obese individuals. These include plantar fasciitis and posterior tibial tendonitis, which can both become chronic. The reduced mobility from foot pain can also decrease your quality of life, make it more difficult to exercise, and lead to further weight gain.
Obesity is also associated with a host of systemic health complications that can affect the feet. Obese people may be more at risk of developing gout and arthritis, which damage the joints. There is also an increased risk of diabetes and poor circulation. Together, these conditions can lead to the development of diabetic foot wounds, which heal slowly and poorly and can cause serious health complications should they become infected.
Making healthy lifestyle changes is one way to prevent the foot problems associated with obesity. Reduce weight (and the risk of gout) by eating a healthy diet and exercising. Wear shoes that fit properly and support your feet. Your chiropodist may suggest orthotics, medications, or other treatments to address any foot pain and to improve your overall mobility and quality of life. To learn more, consult with a chiropodist near you.
Several Kinds of Arthritis
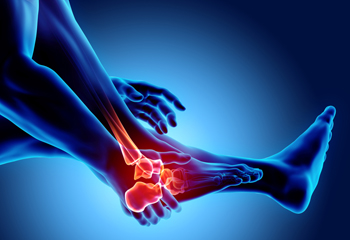
Some of the symptoms that are associated with arthritis are severe pain and inflammation. There are different types of arthritis, and osteoarthritis is considered to be the most common. It can affect the cartilage lining of the joints in the feet and generally causes stiffness, possibly making it difficult to walk. Women are more likely to develop rheumatoid arthritis than men, and pain and swelling often accompany this type of ailment. It is said that men are more likely to be affected by the type of arthritis that is known as gout and the discomfort from this condition can be debilitating. It affects the joint in the big toe and can develop from an excess amount of uric acid in the bloodstream. If you have any of the above symptoms and it becomes difficult to complete daily activities, it is strongly advised that you confer with a chiropodist who can provide arthritic foot care treatment.
Osteoarthritis in the feet or ankles can be a painful and disabling condition that may interfere with your daily activities. If you have arthritis, please consult with one of the chiropodists from The Footcare Centre. Our chiropodists will assess your condition and provide you with quality foot and ankle treatment.
What Is Osteoarthritis?
Osteoarthritis is a condition in which the protective layer of cartilage in the joints breaks down over time. This loss of cartilage causes the bones to rub together during movement, leading to pain and inflammation. Osteoarthritis is associated with aging, and often affects the small joints of the feet and ankles.
Symptoms
Symptoms of osteoarthritis include:
Joint pain
Joint stiffness
Swelling in or around the joint
Restricted range of motion
Difficulty walking
Diagnosis
Osteoarthritis can be diagnosed through physical examination. You may also need to have an X-ray taken to assess the extent of the damage caused by arthritis.
Treatment
Treatment for osteoarthritis focuses on reducing symptoms and improving the function of the affected joints. Conservative treatments include oral pain medications, orthotic devices, bracing or immobilizing the affected foot or ankle, steroid injections into the affected joint to reduce inflammation, and physical therapy. In more severe cases, surgery may be necessary.
If you have any questions, please feel free to contact our office located in . We offer the newest diagnostic and treatment technologies for all your foot care needs
Arthritic Foot Care
Osteoarthritis is a condition in which the cartilage located on the ends of joints deteriorates over time. Cartilage is very important, as it protects and cushions the bones during movement. Osteoarthritis is the most common type of arthritis and is associated with aging. It can affect any of the joints in the body, and frequently affects the joints of the feet and the ankles. Though rarer, osteoarthritis can also occur as a consequence of an injury, such as as a sprain or fracture, or as a result of abnormal foot biomechanics.
Symptoms of osteoarthritis include pain and stiffness in the joints, swelling, and difficulty walking or bending the joints. In some cases, bony protrusions called bone spurs can develop on the affected joints. Osteoarthritis is a progressive condition, meaning that it worsens over time. Diagnosing the condition early allows for earlier treatment, which can help preserve the health and function of your joints.
A variety of treatment options are available for osteoarthritis. Pain can often be minimized by taking nonsteroidal anti-inflammatory medications, getting steroid injections into the affected joints, and wearing orthotics. Bracing or immobilizing the affected foot or ankle may help reduce inflammation and prevent deformity of the joint. Doing specific exercises can help strengthen the muscles in the feet and ankles to prevent injuries. In cases where more conservative treatments have failed or in which arthritis has progressed significantly, surgery may be an option. If you have osteoarthritis in your feet or ankles, it is recommended that you consult with a chiropodist.
Why Is My Toenail Black?

If you notice that your toenail has turned black, it is a sign that you may need a new pair of running shoes. Running too far for too long is a primary cause of black toenail, causing a soft tissue injury. Black toenails are common among long-distance runners and soldiers who march a long way in boots. A blackened toenail is caused by a subungual hematoma, or bleeding under the toenail, often called a jogger's toe. The main cause is continued rubbing inside the shoe, but may also be the result of dropping something heavy on your toe. Symptoms include a blackened appearance of the nail, a feeling of throbbing pain, and in some cases the loosening of the nail from the bed. The blood collects under the toenail, causing the black appearance, and pressure causes the pain. Treatment for black toenails includes draining the blood from under the nail or removing the nail. If you have developed a black toenail, please see a chiropodist for an examination and treatment options.
Injuries to the foot and ankle are very common among athletes. If you have experienced an injury, please consult with one of the chiropodists from The Footcare Centre. Our chiropodists will assess your condition and provide you with quality foot and ankle treatment.
Common Injuries Among Athletes:
Achilles tendon injuries
Ankle strains or sprains
Plantar fasciitis
Fractures
Turf toe
Joint dislocations
Sever’s disease
Morton’s neuroma
Symptoms
Symptoms will depend on the cause and severity of the injury. Common symptoms for a foot or ankle injury include pain, swelling, tenderness, bruising, a reduced range of motion, and difficulty bearing weight or walking on the affected foot or ankle.
Diagnosis
Sports injuries are typically diagnosed after carefully examining the affected foot or ankle. This includes moving the injured area to test its range of motion. Medical history will need to be provided, as well as detailed information about how the injury occurred. Imaging studies, such as X-rays or MRIs, may be used to confirm or rule out certain diagnoses.
Treatment
Just like symptoms, treatment will depend on the type of injury and its severity. Initial treatment for many sports injuries is aimed at controlling inflammation and promoting the healing response. The acronym R.I.C.E is a helpful guide to implement for most acute injuries. This method involves resting, icing, compressing, and elevating the affected foot or ankle. In addition, anti-inflammatory medications may be administered and orthotic devices may be prescribed. For more severe injuries, surgery may be required. Lastly, rehabilitation or physical therapy may be needed to gain full functionality in the afflicted area.
If you have any questions, please feel free to contact our office located in . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Reasons Bunions Can Develop

The location on the foot where a bunion generally develops is the bottom of the joint in the big toe. It can happen due to genetics, or if an injury has occurred. The bony protrusion of a bunion that develops in this area may cause the big toe to shift toward the other toes, and the foot may look deformed. Many patients have to purchase larger shoes to accommodate the shape of the foot. Additionally, walking may be uncomfortable, and limping may help to alleviate the discomfort. Mild relief may be found when the affected foot is soaked in warm water, and it may help to wear a protective pad over the bunion. Effective prevention methods of bunions can include avoiding wearing high heels, wearing shoes with bigger toe areas, and by developing strength in the feet with a routine exercise regime. If you have developed a bunion, it is advised that you schedule an appointment with a chiropodist who can effectively treat this condition.
Bunions progressively worsen over time and may cause walking in your shoes to become difficult. To learn more about bunions, please consult with one of the chiropodists from The Footcare Centre. Our chiropodists will assess your condition and provide you with quality foot and ankle treatment.
What Are Bunions?
A bunion is a bony bump that protrudes from the base of the big toe. Bunions are caused due to a misalignment of the first metatarsal. The characteristic bump of a bunion forms when the metatarsal shifts outwards from its proper position. Bunions develop slowly over time and progressively worsen without treatment. The skin over the bunion may develop calluses due to the friction from shoes. Eventually, a bunion can make walking uncomfortable or even painful. Bunions are one of the most common foot deformities and are especially common in women and older adults.
Symptoms
A bunion appears as a bulging bump on the outside of the base of the big toe.
The bunion may also:
Be swollen, red, or sore
Develop corns or calluses over it
Cause pain
Limit the big toe’s range of motion
Treatment
There are several different treatments available for bunions. Conservative treatment options include wearing shoes with a wider toe box, cushioning the bunion with a specialized pad, wearing shoe inserts, icing the bunion if it becomes inflamed, and taking medications to relieve pain. In more severe cases, more invasive procedures may be done. This may involve removing the swollen tissue around the bunion, straightening the big toe, realigning the bones at the front of the foot, or a combination of these procedures.
If you have any questions, please feel free to contact our office located in . We offer the newest diagnostic and treatment technologies for all your foot care needs
Bunions
A bunion is a bony bump that develops on the outside of the big toe, at the base of the big toe joint. Over time, a bunion can cause the big toe to move out of its proper alignment and lean towards the second toe. The bunion may become painful, stiff, red, and swollen. Calluses sometimes form on top of the bunion as the bunion rubs against the inside of your shoe as you walk. Calluses can also form on the area where your big toe rubs against your second toe, or on the ball of the foot.
Bunions are extremely common, especially in older adults and women, although children can develop bunions or, in very rare cases, be born with them. What exactly causes bunions is unclear. They may occur as a result of a genetic predisposition due to the shape and structure of the foot or because of one’s gait. Wearing shoes that are too tight, have excessively high heels, or narrow, pointed toes may contribute to the development of bunions. Certain medical conditions, such as arthritis and flat feet, may make bunions more likely as well.
Bunions can be treated through conservative methods such as switching the shoes that you wear for shoes that are wider and more comfortable, wearing custom orthotics, wearing pads placed over the bunion to reduce pain, taking nonsteroidal anti-inflammatory medications, and icing the foot. When conservative treatments are not effective, invasive procedures may be recommended. For more information about bunions, please consult with a chiropodist.
Diabetic Foot Ulcers

Anyone with diabetes may be at a higher risk of developing foot ulcers. They are usually caused by sores or wounds that do not heal properly and spread beneath the skin to the soft tissue and muscle sheaths below. A diabetic who has developed peripheral neuropathy often loses the feeling in the toes and feet. Because a sore or minor cut can’t always be detected, particularly if it is on the bottom of the foot, it may form an ulcer. Symptoms of diabetic ulcers include discoloration of the skin or toenails, pain and redness, swelling, pus or fluid discharge, and a foul odor coming from the foot. The most common treatment is debridement, a process that removes dead tissue. It is strongly suggested that you not do this on your own, but consult a chiropodist, who can conduct the process in a safe and hygienic way. Afterward, you may be directed to wear special shoes or use crutches or a wheelchair until the wound heals completely. It is also suggested to avoid walking barefoot and make sure the wounded area is kept clean.
Diabetes can cause serious problems in the lower limbs if proper preventive measures are not taken and diabetic wound care is not performed. If you would like to learn more about caring for diabetic feet, please consult with one of the chiropodists from The Footcare Centre. Our chiropodists can help you maintain the health of your lower limbs and your mobility.
Diabetes can lead to a host of foot and ankle complications, including:
Poor circulation
Peripheral neuropathy
Diabetic foot wounds and ulcers
Infection
Corns and calluses
Dry, cracked skin
Nail disorders
Hammertoes
Bunions
Charcot foot
If you have diabetes, you must be vigilant of any changes in your foot health. This is best done through daily foot inspections. Using a mirror to help you if necessary, look for any:
Cuts, scrapes, sores, or wounds
Bruising or discoloration
Swelling
Rash
Foul odor
Nail changes
Hair loss
Warmth and inflammation
Deformities
Lower limb pain
Strange sensations (numbness, tingling, burning, pins, and needles)
If you detect anything unusual, seek the care of a chiropodist as soon as possible. If you have any questions, please feel free to contact our office located in . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Diabetic Foot Care
Though diabetes begins with the pancreas not producing enough insulin, thus raising your blood sugar levels, it is a systemic condition that can affect every part of your body. The feet are no exception, and a variety of lower limb problems are very common among people with diabetes.
One of the primary foot-related concerns for patients with diabetes is diabetic foot ulcers (DFUs). These are poorly healing open wounds on the feet that are at high risk of becoming infected due to a weakened immune system, another common complication of diabetes. Nerve damage in the feet caused by high blood sugar levels interferes with pain signaling between the peripheral nerves in the feet and the central nervous system (the brain and spinal cord). When this signaling is disrupted, it can be difficult to detect foot injuries, such as cuts and scrapes, when they occur. These injuries are then left unnoticed and untreated until they have significantly worsened. Poor circulation, another complication of diabetes, means that not enough nutrients reach the feet. Without them, the wounds on the feet heal slowly and poorly, or not at all. These wounds can then become infected, leading to tissue death.
The best way to prevent DFUs and their consequences is to carefully monitor the health of your feet through daily foot inspections. Using a mirror to help you see your feet fully, look for any cuts, scrapes, sores, bruising, swelling, discoloration, rashes, hair loss, deformities, or nail changes. Take note of any foul odors, pain, warmth, and strange sensations such as numbness, tingling, burning, or pins and needles. If you notice a problem, seek the care of a chiropodist as soon as possible. Early treatment is key to avoiding potential complications.
DFUs are not the only foot problem diabetics are more likely to encounter. Diabetes can also increase your risk of corns and calluses, cracked skin, bunions, hammertoes, Charcot foot, nail disorders, and various infections. If you have diabetes, it is strongly suggested that you are under the care of a doctor who can help you monitor your foot health, treat any existing conditions, and prevent future ones.
Taking Care of Foot Blisters
A blister is a pocket of fluid that forms on the skin, including the skin of the feet. There are many causes of foot blisters. They generally arise from rubbing or friction from poor fitting shoes or socks or long periods of being on the feet – walking, standing, or exercising. Foot blisters can become painful and interfere with daily functioning. Typically, one can treat a blister at home by simply covering it with a Band-aid to help protect the sore. It should eventually harden and disappear. Long-term, make sure to wear shoes and socks that fit properly and do not rub or constrict the foot in any way. If a blister on your foot does not heal in a relatively short period of time, or if you develop other symptoms (such as a fever, nausea, and chills), it is wise to consult with a chiropodist to make sure it has not become infected and to obtain suggestions for proper treatment protocols.
Blisters can usually be treated at home, however, if you have recurring blisters or experience significant discomfort or pain, please consult with one of the chiropodists from The Footcare Centre. Our chiropodists will assess your condition and provide you with quality foot and ankle treatment.
What Is a Blister?
A blister is a small pocket of fluid in the upper skin layers and is one of the body’s natural responses to injury or pressure. Blisters can also result from burns, fungal or viral skin infections, and the feet are particularly prone due to ill-fitting footwear and friction. Friction on the skin causes the upper layer of skin to separate from the lower layers. The space that this separation creates then becomes filled with a liquid called serum, which protects the lower layers of skin.
Treatment
If you notice a blister on your foot, you can cover it with a soft bandage or dressing to protect it. Popping the blister is discouraged. Doing so exposes the raw skin underneath it to bacteria and also raises the risk of infection. If a blister pops naturally, let it drain before covering it with a bandage. Blisters usually heal on their own or with home treatment, however, if your blister is recurring, very painful, or appears infected, it is recommended that you see a chiropodist for treatment.
Prevention
You can help to prevent blisters by wearing comfortable, well-fitted shoes. Keep your feet dry by wearing moisture-wicking socks and dust your feet with talcum powder if they tend to get sweaty. If you have areas on your feet that are more susceptible to blisters, you might be able to prevent the blister from forming by covering it with a pad.
If you have any questions, please feel free to contact our office located in . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters
Blisters are fluid-filled bubbles of skin that can appear on any part of the body and are particularly common on the feet. Most foot blisters form due to friction. As you walk, run, or go about your daily activities, your shoes may rub against specific areas of your feet, causing the skin to become damaged. The top layer of skin then separates from the lower layers of skin. The area between the separated layers fills with a fluid called serum, whose purpose is to cushion and protect the raw skin below the blister.
If you find a friction blister on your foot, it is highly recommended that you do not pop it. Popping the blister drains the fluid inside of it and exposes the raw skin underneath, increasing your risk of infection. Instead, protect the blister by loosely covering it with a bandage. You can also use special padding around the blister to protect it. Typically, friction blisters naturally heal over the course of one to two weeks. Friction blisters can be prevented by wearing well-fitted shoes and moisture-wicking socks. Wearing soft bandages over areas of your foot that tend to blister may also help.
Sometimes foot blisters can be caused by problems other than friction. Blisters can develop due to a sunburn, frostbite, or exposure to an allergen, as well as from medical conditions such as fungal infections or eczema. If you frequently find blisters on your feet, it is recommended that you consult with a podiatrist.






